Aside
-
Diseases & Conditions
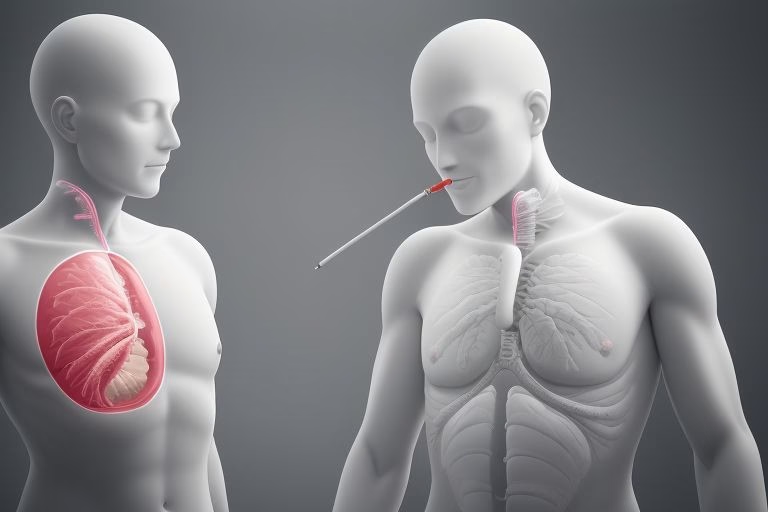
7 Incredible Lung Cancer Statistics in the United States That Will Inspire You to Act Now!
Lung cancer statistics in the united states have been a hot topic among health professionals, researchers and the general public…
Read More » -
Lifestyle

7 Amazing Strategies to Eliminate Ear Pimples: Uncover why do i get pimples inside my ear and Enjoy Clear, Confident Ears!
Have you ever wondered why do i get pimples inside my ear? If you’re tired of dealing with these annoying…
Read More » -
Lifestyle

10 Amazing Ways to Beat dandruff in beard: Achieve a Dapper, Flawless Look Today!
Having a well groomed beard is not just about looking stylish, its also about feeling confdent and taking care of…
Read More » -
Diseases & Conditions

10 Incredible Reasons to Act Now: Can A Gum Infection Kill You?
Are you wonderin if a gum infection can kill you? In todays fast paced world, many of us overlook the…
Read More » -
Fat Burning

10 Unbelivable Ways to Boost Your Health with the best protein for women Today!
When it comes to nurturing your body and energising your daily routine, finding the best protein for women can make…
Read More » -
Diseases & Conditions

10 Incredible Pressure Points for Clogged Nose Relief Techniques That Will Brighten Your Day
If yer fed up with that stuffy nose making every breath a struggle, you’re in the right place! In this…
Read More » -
Fat Burning

10 Amazing Ways to Lose Belly Fat on a Man and Boost Your Confidence!
If you’re looking for surefire ways how to lose belly fat on a man and reclaim your health, then you’ve…
Read More » -
Diseases & Conditions

7 Amazing Bed Bug Freeze Treatment Tips for a Bug-Free Home
Are you fed up with those pesky bed bugs invading your space? If so, you’re not alone! Millions of people…
Read More » -
Diseases & Conditions

10 Incredible Facts: Why steven johnson syndrome curable Offers New Hope for Recovery!
Stevens Johnson syndrome, often mispelled as “steven johnson syndrome curable,” is a rare yet life-altering condition that many people have…
Read More » -
Diseases & Conditions

10 Incredible Reasons Why what causes blindness Isn’t The End: A Positively Life-Changing Guide
When it comes to what causes blindness, many peope are left confused and worried. But this comprehensive guide is here…
Read More »