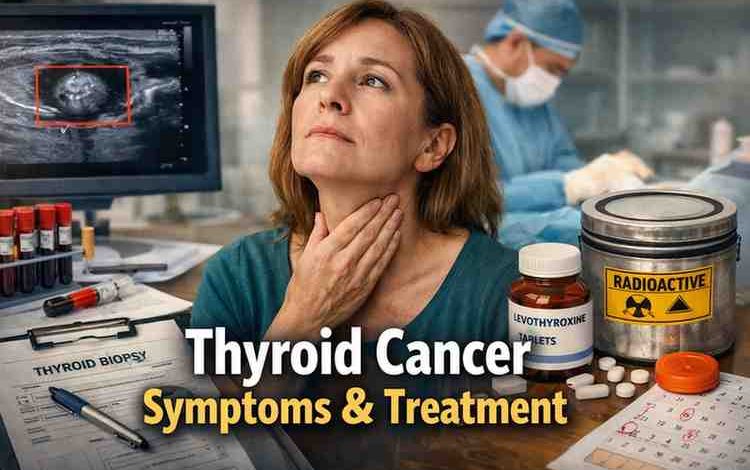
I’ve watched more than a few people freeze the moment they hear the word “thyroid.”
Not because they know what it means.
But because they don’t.
It usually starts small. A lump someone feels in the mirror. A routine physical where a doctor pauses just a second too long. Or weird symptoms that don’t quite add up — fatigue that feels deeper than normal, voice changes, something slightly off when swallowing.
And then comes the spiral.
Most people start Googling “Thyroid Cancer Symptoms and Treatment” at 11:47 PM. I know because they’ve told me. They’re half panicked. Half numb. And honestly? Usually misinformed.
From what I’ve seen, the fear is often bigger than the reality — but the confusion is very real.
Let me walk you through what I’ve consistently observed across real cases. The good. The hard parts. The stuff nobody explains well.
The First Pattern: Most People Don’t Feel “Sick”
This surprised me after watching so many people go through testing.
Almost everyone assumes cancer must feel dramatic. Painful. Obvious.
Thyroid cancer usually isn’t.
In fact, most people I’ve worked with mess this up at first — they dismiss symptoms because they feel mostly normal.
Here’s what I’ve seen show up repeatedly:
-
A painless lump in the front of the neck
-
Slight voice hoarseness that lingers
-
Trouble swallowing that feels subtle
-
Swollen lymph nodes
-
A feeling of “tightness” in the throat
Fatigue sometimes shows up. But it’s messy. Hard to pin down.
The thyroid sits low in the neck. Small gland. Controls metabolism. When something grows there, it doesn’t always scream.
And that’s why early detection often happens by accident.
What People Usually Get Wrong About Thyroid Cancer Symptoms
I didn’t expect this to be such a common issue, but almost everyone I’ve seen struggle with this does this one thing wrong:
They assume symptoms must match Google’s worst-case scenario.
So they either:
-
Panic over mild symptoms that aren’t cancer
-
Or ignore quiet signs because they’re not dramatic enough
The middle ground? That’s where clarity lives.
From what I’ve seen:
-
Pain is rare early on
-
Weight changes are not always connected
-
Thyroid function tests can be completely normal even if cancer is present
That last one throws people off.
Thyroid cancer doesn’t always disrupt hormone production.
Which means blood work can look fine. And that creates false reassurance.
The Types Matter (But Not in the Way You Think)
In the U.S., most thyroid cancers fall into a few main categories:
-
Papillary (most common)
-
Follicular
-
Medullary
-
Anaplastic (rare but aggressive)
What I’ve consistently seen:
Papillary thyroid cancer is by far the most common. And it’s usually slow growing.
This is where relief comes in for many people.
When someone hears “cancer,” they expect worst-case timelines.
But papillary thyroid cancer has one of the highest survival rates of any cancer. Especially when caught early.
That said.
“High survival rate” doesn’t mean “emotionally easy.”
I’ve seen people struggle more with uncertainty than with physical recovery.
Let’s Talk Treatment — What Actually Happens
When people search “Thyroid Cancer Symptoms and Treatment,” what they really want is this:
What will they do to me?
Here’s the real-world flow I’ve observed most often in U.S. healthcare settings:
Step 1: Ultrasound
If a lump is found, imaging comes first.
Step 2: Fine Needle Biopsy
This scares people more than it should. It’s uncomfortable. Quick. Usually outpatient.
Step 3: Surgery
If cancer is confirmed, surgery is the primary treatment.
Options usually include:
-
Lobectomy (removing part of thyroid)
-
Total thyroidectomy (removing entire gland)
Most people I’ve watched go through this are shocked at how fast the surgical phase moves.
Diagnosis → surgery can feel like a blur.
Recovery: The Part Nobody Explains Well
Here’s what surprised me after watching dozens of cases.
The physical recovery from surgery is often smoother than the emotional recovery.
Most people:
-
Go home same day or next day
-
Have mild to moderate soreness
-
Heal visibly within 2–3 weeks
But emotionally?
Different story.
People wrestle with:
-
“Did we get all of it?”
-
“What if it comes back?”
-
“Will I feel normal again?”
That part lingers.
Radioactive Iodine: Who Actually Needs It?
This is where confusion explodes.
Not everyone needs radioactive iodine (RAI) treatment.
From what I’ve seen:
-
Small, low-risk cancers often skip RAI
-
Larger tumors or spread to lymph nodes may require it
RAI works because thyroid cells absorb iodine. The radioactive version targets leftover cells after surgery.
What most people misunderstand:
It’s not chemotherapy.
Side effects vary but often include:
-
Dry mouth
-
Temporary taste changes
-
Mild fatigue
Isolation for a few days is required because of radiation safety.
That part feels strange for most people.
Hormone Replacement: The Long Game
If the entire thyroid is removed, lifelong thyroid hormone medication becomes necessary.
Usually levothyroxine.
And here’s where almost everyone I’ve seen struggle with this does this one thing wrong:
They assume the first dose will be perfect.
It rarely is.
Finding the right dosage can take:
-
6–12 weeks between adjustments
-
Multiple blood tests
-
Patience most people don’t expect to need
During this time, people can feel:
-
Too wired
-
Too tired
-
Slightly “off”
This phase tests patience more than anything.
But once stabilized? Most people return to very normal lives.
How Long Does Treatment Take?
Short answer:
-
Surgery recovery: 2–3 weeks
-
Hormone stabilization: 2–6 months
-
Full emotional adjustment: honestly? 6–12 months
This varies.
But from what I’ve seen, most people feel like themselves again within a year.
Not overnight. Gradually.
Common Mistakes I’ve Seen Repeated
Let me be direct here.
These are patterns:
-
Ignoring small neck lumps for months
-
Doctor shopping for reassurance instead of clarity
-
Obsessively reading worst-case stories online
-
Skipping follow-up scans because “I feel fine”
-
Expecting medication adjustments to feel instant
That third one? It’s brutal.
The internet overrepresents rare complications.
Most real-world cases are far more manageable than what shows up in dramatic forum threads.
Is Treatment Worth It?
This question comes up more than people admit.
Especially for small, slow-growing cancers.
Some U.S. providers even recommend active surveillance for very tiny papillary cancers.
So is treatment worth it?
From what I’ve seen:
-
For larger or spreading cancers — yes, absolutely.
-
For tiny, contained cancers — it depends on patient comfort and medical advice.
The emotional toll of “watch and wait” can be heavier than surgery for some people.
Others prefer avoiding surgery if possible.
There’s no universal right answer.
But indecision tends to increase anxiety more than action.
Who Will Struggle Most With This Process?
Honestly?
People who:
-
Need certainty immediately
-
Have high anxiety around health
-
Struggle with medication adherence
-
Expect fast, dramatic recovery
This is a slow-burn experience.
Not chaotic. But steady.
FAQ: Direct Answers People Ask
What are early thyroid cancer symptoms?
Often a painless neck lump. Sometimes hoarseness or swallowing difficulty. Many people have no obvious symptoms.
Is thyroid cancer curable?
Most papillary and follicular thyroid cancers have very high survival rates when treated early.
Will I need chemotherapy?
Rarely. Surgery and sometimes radioactive iodine are the primary treatments.
Can you live without a thyroid?
Yes. With proper hormone replacement, most people live normal lives.
Does thyroid cancer spread quickly?
Most common types grow slowly. Anaplastic thyroid cancer is aggressive but rare.
Objections I Hear All the Time
“What if surgery changes my voice permanently?”
It’s possible but uncommon in experienced surgical hands. Temporary hoarseness is more typical.
“I don’t want to take medication forever.”
I get it. But many people I’ve seen adjust to levothyroxine as part of routine life — like brushing teeth.
“What if it comes back?”
Follow-ups are designed to catch recurrence early. Monitoring is structured and predictable.
Reality Check Section
This isn’t a light experience.
Scans trigger anxiety.
Blood test days feel tense.
Waiting for pathology results? Brutal.
Even with high survival rates, the word “cancer” hits hard.
And sometimes hormone balance never feels 100% identical to before.
Most people adapt.
But adaptation takes time.
Practical Takeaways
If I had to summarize what consistently works:
-
Don’t ignore a neck lump
-
Get an ultrasound before panicking
-
Choose an experienced endocrine surgeon
-
Expect hormone dose adjustments
-
Protect your mental health during monitoring
And emotionally?
Expect waves.
Some days you’ll feel fine. Other days you’ll spiral for 20 minutes. That’s normal.
Patience looks like:
-
Taking meds at the same time daily
-
Showing up for labs
-
Not catastrophizing every sensation
Small discipline. Over time.
I won’t pretend thyroid cancer is “no big deal.”
But I’ve watched enough people walk through Thyroid Cancer Symptoms and Treatment to know this:
It’s rarely the monster people imagine at midnight.
It’s structured. Manageable. Often highly treatable.
Still scary. Still emotional.
But not hopeless.
And sometimes the real relief comes not from perfect outcomes —
but from finally understanding what’s actually happening.