Living with ulcerative colitis can feel overwhelming—but knowing exactly what type of UC you have can change everything. Whether you’ve just been diagnosed or have been dealing with symptoms for years, understanding the types of ulcerative colitis is the first step toward getting real relief.
In this guide, we break down the 7 major types of ulcerative colitis—what they are, how they affect your body, and the best ways to manage them. Let’s dive into it.
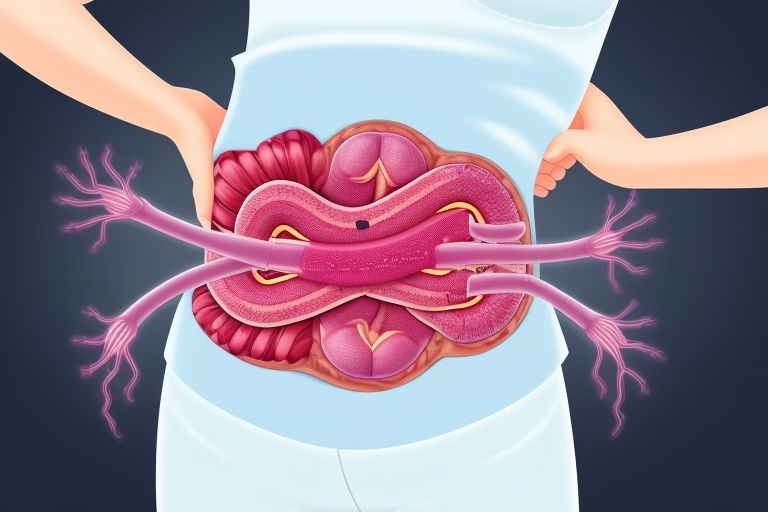
What Is Ulcerative Colitis? (UC)
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that causes inflammation and ulcers in the lining of the colon and rectum. It can lead to painful symptoms, including abdominal cramps, diarrhea, fatigue, rectal bleeding, and weight loss.

Unlike Crohn’s disease, which can affect any part of the digestive tract, ulcerative colitis only affects the large intestine. The severity and symptoms vary depending on the type you have.
Why Knowing Your Type of UC Matters
Understanding the specific type of ulcerative colitis helps your doctor tailor your treatment plan. Some types respond better to certain medications, while others may require lifestyle changes or even surgery. When you know your UC type, you can take back control of your health.
🔍 The 7 Main Types of Ulcerative Colitis
1. Ulcerative Proctitis
This is the mildest form of UC, where inflammation is limited to the rectum (the last part of the colon).
Key Symptoms:
-
Rectal bleeding
-
Urgency to have bowel movements
-
Mild abdominal discomfort
-
Feeling of incomplete evacuation
Who’s Most at Risk?
People in their 20s to 40s, but it can affect anyone at any age.
Treatment Options:
-
Topical suppositories
-
Anti-inflammatory medications like mesalamine
-
Lifestyle changes (e.g., increased fiber, hydration)
Ulcerative proctitis may seem less serious, but early treatment can prevent progression to more severe forms of colitis.
2. Proctosigmoiditis
In this type, inflammation affects both the rectum and the sigmoid colon (the lower part of the colon).
Symptoms to Watch:
-
Diarrhea with blood
-
Cramping in the lower abdomen
-
Pain during bowel movements
-
Mucus in stool
Treatment:
-
Mesalamine enemas or oral meds
-
Corticosteroids if inflammation worsens
-
Diet low in processed foods and high in anti-inflammatory nutrients
👉 A good resource to learn more about this type is Crohn’s & Colitis Foundation.
3. Left-Sided Colitis (Distal Colitis)
Inflammation extends from the rectum to the splenic flexure (the bend near the stomach on the left side).
Common Signs:
-
Loss of appetite
Treatment Options:
-
5-ASA drugs (like sulfasalazine)
-
Biologics (for moderate to severe cases)
-
Anti-diarrheal medication and iron supplements
This form can significantly impact your daily life, so sticking to your treatment plan is essential.
4. Pancolitis (Extensive Colitis)
This is a more severe form where the entire colon is inflamed. It often leads to intense symptoms and higher complication risks.
Severe Symptoms Include:
-
Profound weight loss
-
Severe fatigue
-
Persistent bloody stools
-
Fever and night sweats
-
Increased risk of colon cancer
Treatment Must-Haves:
-
Biologic therapies (e.g., infliximab)
-
Immunosuppressants
-
Surgery (in extreme cases)
💡 Tip: Stay consistent with your screenings and colonoscopies to monitor long-term risks.
Learn more about extensive colitis and treatment trials at ClinicalTrials.gov.
5. Fulminant Colitis
This is the most dangerous and life-threatening form of ulcerative colitis. It develops rapidly and demands immediate medical attention.
Emergency Symptoms:
-
Severe dehydration
-
Uncontrolled diarrhea
-
Shock or confusion
-
Risk of toxic megacolon
-
High fever and pain
Urgent Treatment Needed:
-
Hospitalization
-
IV fluids and steroids
-
Possibly colectomy (removal of colon)
Fulminant colitis is rare but serious. If you suspect you have it, go to the ER immediately.
6. Backwash Ileitis
Although UC usually doesn’t affect the small intestine, backwash ileitis refers to inflammation that spills over into the ileum (the end of the small intestine).
Signs You May Have It:
-
Diarrhea that worsens
-
Nausea
-
Bloating
How It’s Managed:
-
Biologic medications
-
Close monitoring with imaging and endoscopy
-
Adjustments in diet (e.g., low FODMAP)
This type often co-exists with pancolitis, making it even more important to track your symptoms and triggers.
7. Treatment-Resistant Ulcerative Colitis
This is not a location-based type but a clinical condition where your UC doesn’t respond to standard therapies.
Signs You Might Be Dealing With This:
-
Tried multiple medications with no relief
-
Constant flare-ups
-
Drug side effects outweigh the benefits
Advanced Therapies Include:
-
Biologic infusion treatments
-
Surgical intervention (proctocolectomy)
Want to read success stories of people overcoming treatment-resistant UC? Check out this real patient experience.
How to Know Which Type You Have
Your doctor may recommend:
-
Colonoscopy or sigmoidoscopy
-
Blood tests to check for inflammation markers
-
Stool sample analysis
-
CT scans or MRIs for severe cases
Best Tips to Manage Any Type of UC
Even though each type is different, here are universal strategies to feel better and regain control of your life:
✅ Stick to Your Treatment Plan
Skipping meds often leads to flare-ups. Work with your doctor to adjust dosages or switch medications if needed.
✅ Eat Anti-Inflammatory Foods
Try foods like:
-
Oatmeal
-
Avocados
-
Bone broth
-
Pumpkin and squash
Avoid:
-
Caffeine
-
Spicy foods
-
Processed meats
✅ Keep a Symptom Journal
Log everything—what you eat, how you feel, bowel movement changes, stress levels. It helps spot patterns fast.
✅ Exercise Gently
Yoga, swimming, and walking can improve digestion, reduce inflammation, and boost your mood.
✅ Reduce Stress
Stress triggers inflammation. Practice:
-
Meditation
-
Breathing exercises
-
Spending time outdoors
Explore calming tips from Psychology Today’s wellness blog.
What Triggers UC Flares?
Common UC flare triggers include:
-
Skipping medications
-
Poor diet choices
-
High stress levels
-
Infections or illnesses
-
NSAIDs like ibuprofen
Knowing what sets off your symptoms makes it easier to avoid flare-ups before they start.
When Should You See a Doctor?
If you experience:
-
Persistent bloody stools
-
Severe abdominal pain
-
Night sweats
-
Or if you suspect complications like toxic megacolon…
👉 It’s time to contact a gastroenterologist ASAP.
Early intervention can prevent complications and improve long-term outcomes.
Final Thoughts: Understanding Your UC Type is a Game-Changer
Living with ulcerative colitis doesn’t mean your life is on pause. By identifying your type of UC, you can target treatment, reduce flares, and live a vibrant, fulfilling life.
Each type of ulcerative colitis comes with its own set of challenges, but you’re not alone. With the right info, a supportive healthcare team, and healthy lifestyle choices, you can manage UC like a pro.
Related Reads You’ll Love:
👉 Know someone with UC? Share this article and help them learn the 7 types of ulcerative colitis that could change their life.