
A raw, personal guide to understanding non small cell carcinoma lung cancer from real-life experience, lessons, and honest insights.
Non Small Cell Carcinoma Lung Cancer: A Real, Human Story & Everything I Wish I Knew Earlier
I’ve gotta be honest right from the start — non small cell carcinoma lung cancer (NSCLC) isn’t just another medical phrase to Google and forget. It’s something I lived through pretty closely, and even now, writing this, I can feel a knot in my stomach remembering the hospital smell, the weird beeping machines, and that one doctor who always looked like he wanted to cry with us.
This article isn’t gonna be sterile or robotic.
I’m sharing exactly what I wish someone had told me on day one — when my loved one got diagnosed and my brain basically stopped working.
If you or someone you care about is dealing with NSCLC, I hope this helps you breathe a little easier, understand things better, and maybe avoid some of the mistakes I made (yep, there were a few… more than a few).
Let’s take this step by step.
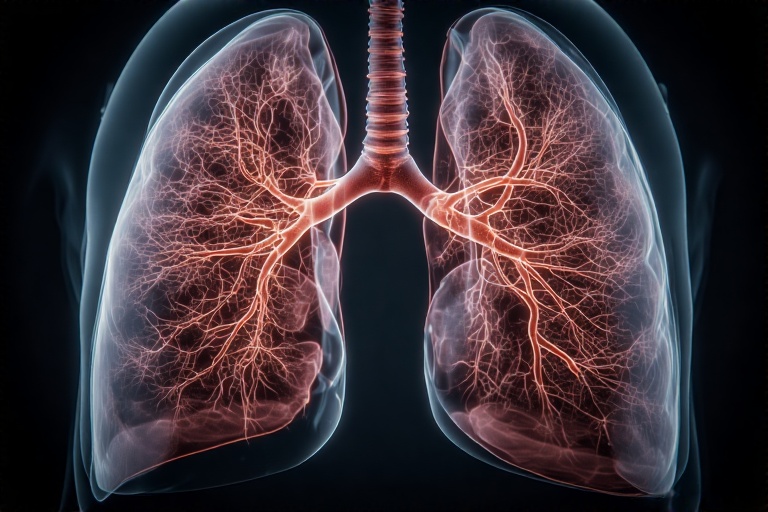
What Exactly Is Non Small Cell Carcinoma Lung Cancer? (Explained Like a Human)
So, the first time the doctor said “non small cell carcinoma lung cancer,” my brain kinda went blank. Too many words. Too much fear. And honestly, the only thing I wanted to ask was:
“Okay… but what do we do now?”
But here’s what I eventually wrapped my head around — in simple, non-medical-student English.
Non Small Cell Carcinoma Lung Cancer (NSCLC) is the most common type of lung cancer. Roughly 80–85% of lung cancer cases fall under this bucket. The “non small” part basically contrasts it with the much more aggressive “small cell” type.
NSCLC grows slower, spreads a bit differently, and often gives doctors more room to work with treatments like:
-
surgery
-
radiation
-
chemotherapy
-
immunotherapy
-
targeted therapy
Now, this does not mean NSCLC is “easy.” Nothing about lung cancer is easy. But it means treatment options are usually a bit broader.
The 3 Main Types (Yep, I Had to Learn These Too)
When you hear “NSCLC,” it’s actually a big umbrella. Doctors often break it down into three main types. At first I thought these were random labels, but they actually change what treatment looks like.
1. Adenocarcinoma
This is the one my relative had. It usually starts in the outer parts of the lungs and is the most common type among non-smokers. (Which, let me tell you, feels like a punch in the gut when you learn it.)
2. Squamous Cell Carcinoma
Starts in the central airways. More common in smokers.
3. Large Cell Carcinoma
A fast-growing type that can appear anywhere in the lung.
I remember scribbling these names in a notebook like a school kid studying for an exam. Except… the stakes were a lot higher.
The Early Signs We Missed (and I Wish We Hadn’t)
Looking back, some symptoms were right in front of us. But life is busy, people brush things off, and honestly — who thinks every cough is cancer?
Here’s what we noticed before the diagnosis:
-
A cough that didn’t go away (I mean months)
-
Tiredness that didn’t match the day’s workload
-
Shortness of breath
-
A little weight loss
-
A weird chest ache that kept getting blamed on “gas”
One of my biggest regrets is pushing things off. I kept saying, “Let’s just wait a week,” and that week eventually turned into three. Not saying this to scare anyone — just being honest.
If there’s one thing I learned, it’s this:
👉 If a cough lasts more than 6–8 weeks, get it checked. Period.
How Diagnosis Actually Works (From Sitting in the Waiting Room to That Phone Call)
The diagnosis process was… a lot. If you’re going through it now, you’re honestly not alone. I sat in so many waiting rooms I could draw the patterns in the chairs from memory.
Here’s how it generally goes:
1. Chest X-Ray
Usually the first red flag.
2. CT Scan
This is where they get a clearer picture. Ours showed a “mass.” That word still haunts me.
3. PET Scan
Checks if the cancer has spread.
4. Biopsy
This is the big one — it’s what confirms non small cell carcinoma.
I remember the moment the doctor said, “It is NSCLC.”
It felt weirdly calm. Like my body went into airplane mode.
Staging: The Part Nobody Warns You About (But You Need to Understand)
This part confused the heck out of me at first.
You’ll hear doctors say: Stage 1, Stage 2, Stage 3A, 3B, Stage 4…
It’s a lot.
Here’s the simple version:
-
Stage 1: Localized. Best case scenario.
-
Stage 2: A bit more spread.
-
Stage 3: More complicated; might involve lymph nodes.
-
Stage 4: Has spread to other parts of the body.
We landed in Stage 3A, which is sort of the “we still have options but it’s gonna be tough” stage.
I remember googling “Stage 3A survival rate NSCLC” at 2 a.m., crying into a pillow so no one would hear. (Yes, it was a bad idea. Don’t do that to yourself.)
Treatment Options (And What They Actually Feel Like in Real Life)
Let me break this down the way someone broke it down for me — in “human language,” not medical jargon.
1. Surgery
If the cancer is still small and in one place, surgery can remove part (lobectomy) or even an entire lung (pneumonectomy).
My cousin had a lobectomy years ago and recovered surprisingly well. They even joked about having “more room in their chest now.” Humor was their coping mechanism.
Not everyone is eligible, though — depends on stage, tumor location, lung function, etc.
2. Radiation Therapy
This one feels like the sci-fi part of cancer care. My relative said it felt tiring more than painful.
Some things we weren’t prepared for:
-
Skin changes (kind of like sunburn)
-
Fatigue that hits like a truck
-
Sore throat if radiation touches that area
But it helped shrink the tumor significantly.
3. Chemotherapy
Chemo is… rough. No way to sugarcoat it.
Nausea, fatigue, hair loss (not always with newer drugs), taste changes — we saw it all.
One day my relative joked, “Food tastes like cardboard dipped in sadness.” We laughed, but it was kinda true.
But chemo also bought us time. And hope.
4. Targeted Therapy
This part felt almost futuristic.
A lot of NSCLC patients have specific gene mutations:
-
EGFR
-
ALK
-
ROS1
-
KRAS
-
BRAF
If you have one of these, targeted therapy can block the cancer’s growth. My relative got tested for mutations (highly recommend doing that early), but didn’t have any targetable ones.
Some people respond amazingly to these meds.
5. Immunotherapy
This was our game-changer.
Immunotherapy basically trains your immune system to attack cancer cells.
We saw a HUGE difference within months — less cough, more energy, even appetite came back.
But we had side effects too:
-
rashes
-
joint pain
-
fatigue
Still, seeing someone get their life back little by little? Worth every side effect.
The Emotional Side (Nobody Prepares You for This Part)
Cancer doesn’t just attack the body — it attacks routines, emotions, even relationships.
Here are some raw truths I learned along the way:
People disappear.
Some friends don’t know how to handle sickness. They drift away. It hurts, but it’s real.
You won’t always be strong.
There were days I was too exhausted to even pretend I was okay.
The patient often hides their pain.
My relative used humor to cope, and I didn’t realize how much they were struggling inside until later.
Little wins matter.
A day with no nausea? A walk without coughing? Those days felt like winning the lottery.
Practical Things I Wish Someone Told Me Earlier
1. Keep a folder (digital or physical).
Medical reports pile up FAST.
2. Ask every doctor: “Can you explain this in simpler words?”
They don’t mind. Trust me.
3. Get genetic testing for mutations early.
It can literally change the entire treatment plan.
4. Don’t ignore mental health.
Therapy, support groups, journaling — they help more than you’d think.
5. Nutrition matters.
Even small snacks help maintain strength. Smoothies were our life-savers.
6. Don’t Google survival charts.
They’re outdated and don’t reflect new treatments.
7. Take pictures, make memories.
Even during treatment. Especially during treatment.
Living With NSCLC (Yes, People Do Live With It)
Something I didn’t know before this journey:
Many people live for years — even with advanced NSCLC.
Immunotherapy, targeted therapies, and better radiation tools have changed everything.
Our oncologist kept reminding us: “We’re not in the cancer era of the 1990s anymore. Treatments are evolving fast.”
And honestly? He was right.
Some days were still awful, but others felt… normal. And that’s something I didn’t think we’d get again.
What I Learned About Hope (And Realistic Optimism)
This might sound cheesy, but here’s the truth:
Hope isn’t pretending everything’s fine.
Hope is waking up and saying, “Okay, let’s deal with today.”
There were moments of joy in the middle of all the chaos — late-night conversations, silly jokes, even arguing over TV shows.
Cancer steals a lot, but it doesn’t get to steal everything.
Conclusion: Here’s My Honest Advice If You’re Facing Non Small Cell Carcinoma Lung Cancer
I’m not a doctor. I’m just someone who went through this with someone I love. So take this for what it is — a deeply human perspective.
Here’s what I’d tell anyone beginning this journey:
-
Ask questions. All of them. Even the “stupid” ones.
-
Don’t skip appointments or scans.
-
Get molecular testing early.
-
Celebrate tiny improvements.
-
Lean on people who show up — not the ones who disappear.
-
Don’t be afraid to feel everything: fear, anger, relief, confusion… it’s all normal.
And most important:
👉 You’re allowed to have hope.
Even on the days it feels impossible.
FAQ (Based on What I Googled at 3 A.M.)
1. How fast does non small cell carcinoma lung cancer grow?
From what doctors explained to me, NSCLC usually grows slower than small cell cancer. But “slow” is still cancer — don’t delay tests or treatment.
2. Can NSCLC be cured?
Early stages? Yes, often with surgery or combined treatments.
Later stages? It may not be “cured,” but many people live years thanks to immunotherapy and targeted meds.
3. Is non small cell carcinoma lung cancer painful?
Pain varies. My relative had chest discomfort early on, but the worst pain actually came from coughing, not the tumor itself.
4. What’s the best treatment for NSCLC?
There’s no universal “best.” It depends on:
-
stage
-
mutations
-
health condition
-
tumor location
Immunotherapy changed everything for us, though.
5. How long can someone live with Stage 3 or 4 NSCLC?
I hesitated to even include this because stats can be terrifying. What I learned is:
modern treatments make those old survival charts pretty useless.
My relative lived far longer than Google predicted.
6. Should caregivers get support too?
YES. Absolutely yes.
You can’t pour from an empty cup, and burnout is real (I learned that the hard way).



