Aside
-
Fashion

10 Amazing Benefits of Keeps Hair Loss Treatment: Your Ultimate Guide to Regaining Confidence
Hair loss can feel overwhelming, but today there’s hope for those seeking a hair loss treatment that really works. In…
Read More » -
Fashion

10 Simple Steps for 2 Month Hair Growth: Unlock Your Luscious Locks in Record Time
Have you ever dreamed of flaunting long, thick, and healthy hair, but felt frustrated with slow progress? If you’re looking…
Read More » -
Diseases & Conditions

7 Incredible Secrets for 1 Year Post Chemo Hair Growth Success
Cancer treatment is a life-altering journey, and while chemotherapy can be daunting, the hope and promise of 1 year post…
Read More » -
Fashion

7 Incredible Secrets to Maximize Anagen Hair Growth for Radiant, Healthy Locks
Are you ready to unlock the full potential of your hair? Discover the transformative power of the anagen hair phase—the…
Read More » -
Fashion

7 Proven Strategies for 1 Year Hair Growth Success: Transform Your Locks Positively!
Achieving 1 year hair growth that is not only long but also healthy hair is a goal for many. Whether…
Read More » -
Fashion

7 Incredible Ways to Enjoy Growing Out Short Hair with Confidence and Style
If you’re ready for a fresh start and an exciting journey, growing out short hair can be one of the…
Read More » -
Fashion

7 Incredible Secrets to Boost Your Average Hair Growth Per Month: Achieve Luscious Locks Naturally
Discovering the secret to vibrant, healthy hair can feel like an endless quest, but the truth is that simple, natural…
Read More » -
Diseases & Conditions
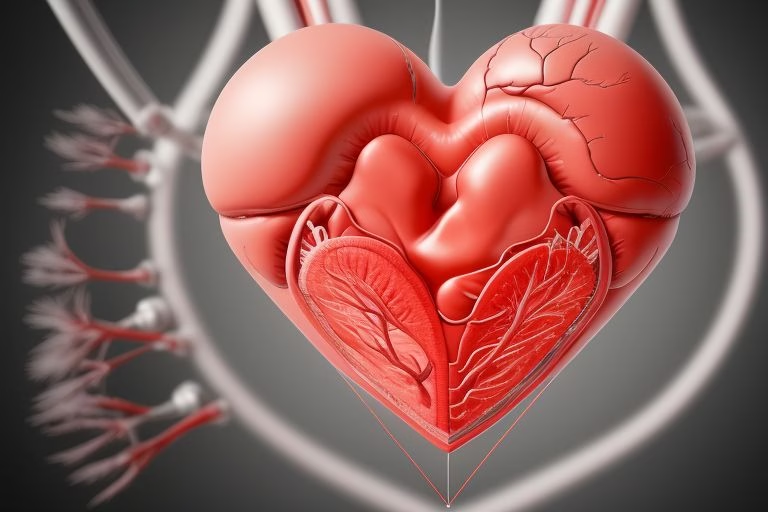
10 Proven Strategies to Improve Ejection Fraction for a Healthier Heart: A Positive Guide
In today’s fast‐paced world, maintaining robust heart health is more important than ever. For those facing challenges related to ejection…
Read More » -
Fat Burning

7 Powerful Secrets for an Obese to Muscular Transformation That Will Change Your Life
Embarking on a journey from obese to muscular transformation is not only about reshaping your body—it’s about reinventing your life.…
Read More » -
Mental Health and Wellness

7 Life-Changing 7 Chakras Meditation Benefits to Transform Your Mind, Body, and Soul
Chakra meditation has been celebrated for centuries as a powerful tool to harmonize our energies, clear blockages, and bring balance…
Read More »