Smallpox Scars: A Guide to Understanding and Treating
Smallpox scars are more than just marks on the skin. They are a testament to the resilience and strength of the human spirit. If you or someone you know has smallpox scars, you may have questions about their appearance, treatment options, and how to embrace and care for your skin. In this comprehensive guide, we will explore the world of smallpox scars, providing valuable insights, practical tips, and relevant information.
Understanding Smallpox Scars
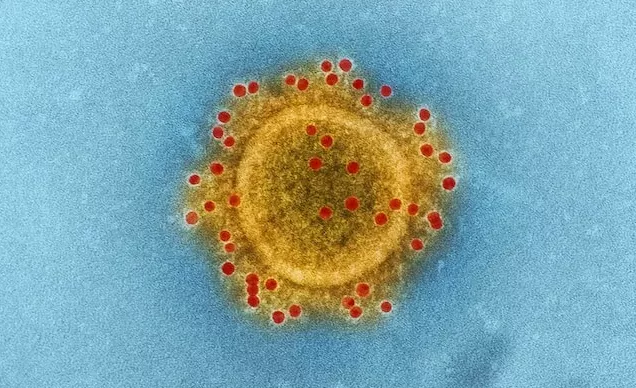
Smallpox scars are caused by the smallpox virus, which can cause a severe rash and other symptoms. The scars typically appear as raised, discolored, and textured skin that can range from white to dark brown. They can also be accompanied by itching, pain, and scarring.
Living with smallpox scars can be a journey of self-discovery and empowerment. It is important to remember that scars are not a source of shame or embarrassment. Instead, they are a source of strength, resilience, and beauty. By embracing your scars, you can empower yourself and inspire others.
Here are some tips for embracing your smallpox scars:
- Celebrate your uniqueness: No two scars are the same. They are unique to you and tell a story about your journey.
- Find beauty in your scars: Scars can be a source of strength and resilience.
- Be proud of your skin: Your skin is your canvas. It is a beautiful and unique part of you.
- Seek support: If you feel self-conscious about your scars, talk to a therapist or counselor. They can help you cope with any emotional distress you may be experiencing.
A Historical Perspective
Smallpox, a highly contagious disease caused by the variola virus, plagued humanity for centuries. It caused severe illness, and survivors were often left with lasting marks on their skin as a result of the scarring caused by the infection.
Types of Smallpox Scars
Smallpox scars can manifest in various forms, including pitted scars, flat scars, or a combination of both. The severity of the scarring depends on factors such as the individual’s immune response and the severity of the infection.
Embracing Your Smallpox Scars
Redefining Beauty Standards
Beauty comes in all forms, and smallpox scars are a testament to the strength and resilience of individuals who have survived the disease. Embracing your smallpox scars is an opportunity to challenge societal beauty standards and celebrate the unique features that make you who you are.
Building Self-Confidence
Developing self-confidence is key to embracing your smallpox scars. Surround yourself with a supportive community, practice positive affirmations, and focus on your inner qualities rather than external appearances. Remember, true beauty radiates from within.
Treating Smallpox Scars
Medical Interventions
Advancements in medical science have provided various treatment options for smallpox scars. Consult with a dermatologist or a skincare professional who specializes in scar management to explore options such as laser resurfacing, microdermabrasion, chemical peels, or dermal fillers.
Home Remedies and Skincare
Complement medical interventions with home remedies and skincare practices that can help improve the appearance of smallpox scars. Examples include applying natural ingredients like aloe vera, lemon juice, or honey to the affected areas. Always consult with a healthcare professional before trying any new treatment.
Caring for Smallpox Scarred Skin
Daily Skincare Routine
Develop a daily skincare routine to nourish and protect your skin. Cleanse gently with a mild, non-irritating cleanser, moisturize regularly to keep the skin hydrated, and use sunscreen with a high SPF to protect against sun damage.
Camouflaging Techniques
If you prefer to minimize the appearance of smallpox scars for specific occasions, explore camouflaging techniques. Use specialized cosmetics such as color correctors, foundations, or concealers to blend the scars with the surrounding skin. Experiment and find techniques that work best for you.
Embracing Support and Community
Connect with Others
Join online communities, support groups, or forums where you can connect with individuals who have similar experiences. Sharing stories, insights, and advice can be empowering and help you navigate the journey of embracing your smallpox scars.
Seek Professional Support
If you’re struggling with the emotional impact of smallpox scars, consider seeking professional support. Therapists, counselors, or support groups specializing in body image issues can provide guidance and strategies for building self-acceptance and confidence.
Smallpox scars carry a historical significance and a personal story of resilience. By understanding, treating, and embracing these scars, we can rewrite beauty standards, cultivate self-confidence, and foster a sense of belonging within supportive communities. Remember, your smallpox scars are a part of your unique journey, and they should be celebrated as symbols of strength. Embrace your skin’s story, care for it with compassion, and let your inner beauty shine through.
Smallpox scars are a part of your story. They are a reminder of your strength, resilience, and beauty. By understanding, treating, and embracing your scars, you can empower yourself and inspire others. Remember, scars are not a source of shame or embarrassment. They are a source of strength, resilience, and beauty.